Practical overview of Einweg E-Zigaretten and health concerns
This comprehensive guide explores disposable vaping devices—commonly referred to in many markets as Einweg E-Zigaretten—and answers a critical public-health question frequently searched: “can e cigarette cause cancer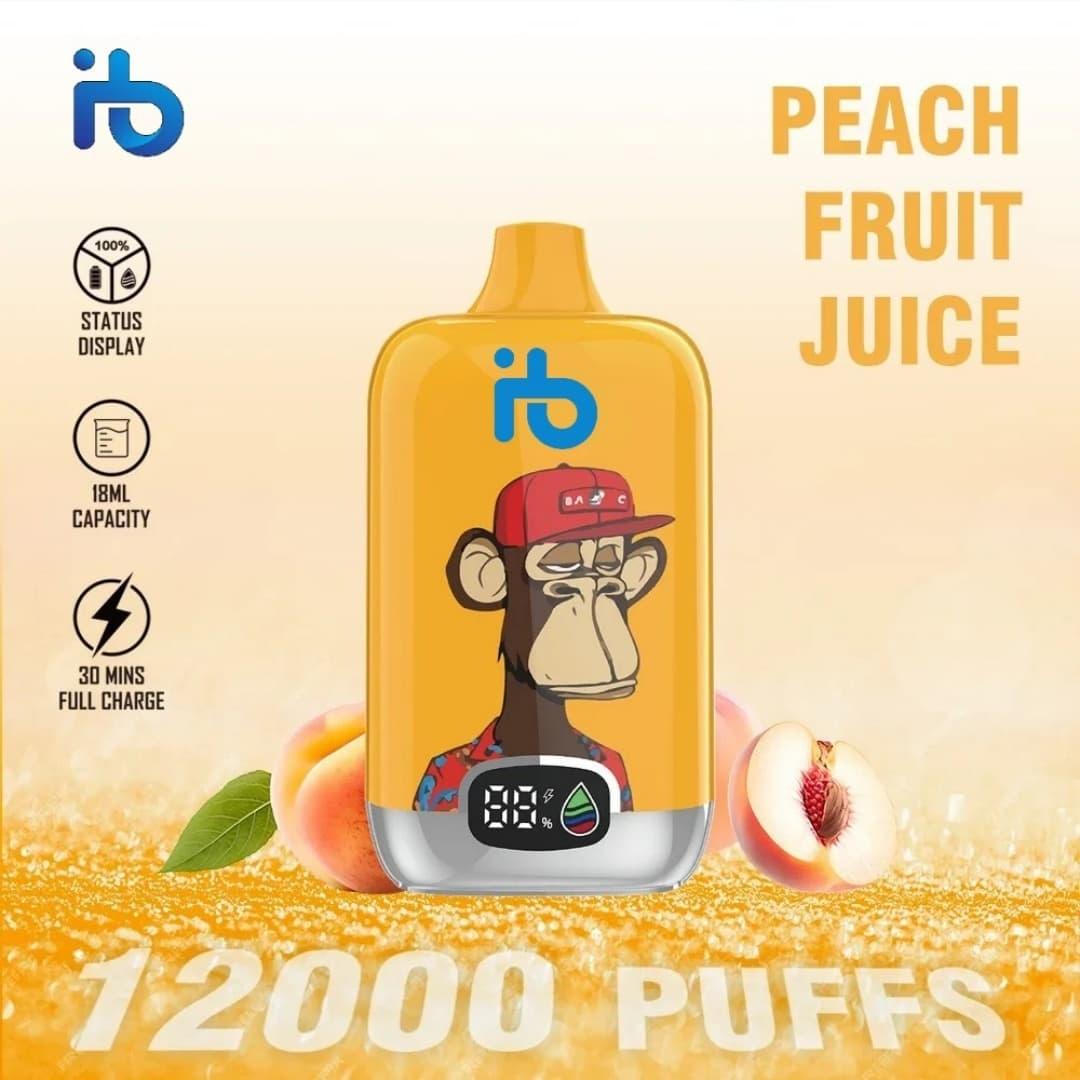 ?” The aim is to provide balanced, evidence-informed guidance for consumers, caregivers, and health professionals who want clear, actionable information. The content below synthesizes device design, chemical composition, toxicology perspectives, epidemiological evidence, practical harm-reduction tips, and regulatory context. It also points to what leading health experts say when asked whether vaping or disposable e-devices increase cancer risk.
?” The aim is to provide balanced, evidence-informed guidance for consumers, caregivers, and health professionals who want clear, actionable information. The content below synthesizes device design, chemical composition, toxicology perspectives, epidemiological evidence, practical harm-reduction tips, and regulatory context. It also points to what leading health experts say when asked whether vaping or disposable e-devices increase cancer risk.
What are disposable vaping devices and why they matter
Disposable or single-use electronic nicotine delivery systems are compact, pre-filled, and throwaway units often marketed for convenience and flavor variety. In many languages and regions they are called Einweg E-Zigaretten, emphasizing single-use design. These devices combine an atomizer, a battery, and a liquid reservoir in a sealed device. Users inhale aerosol generated by heating a nicotine-containing or nicotine-free liquid. Their ubiquity and discreet form factor have led to rapid adoption among adults seeking an alternative to combustible tobacco and among young people exploring flavored products.
Typical components and how they work
- Battery: A small lithium-ion cell delivers power; device safety depends on battery design and protection circuits.
- Heating element: A coil or ceramic heater vaporizes the e-liquid.
- E-liquid: Usually contains propylene glycol (PG), vegetable glycerin (VG), nicotine (optional), flavorings, and other additives.
- Mouthpiece and airflow: Designed for draw activation; some models use mechanical airflow sensors.
Because these devices are pre-filled and disposable, there is no user maintenance, which reduces some user errors but increases waste and raises concerns about quality control, counterfeit products, and unregulated chemical additives.
Key reasons people choose disposable devices
- Convenience and portability.
- Lower upfront cost compared with refillable systems.
- Variety of flavors marketed to adult smokers and sometimes appealing to youth.
- Perceived lower harm compared with burning tobacco—an important reason many adults considering switching cite.
Understanding the primary public-health question: can e cigarette cause cancer
Short answer: The relationship between inhaling e-cigarette aerosol and cancer is complex. While e-cigarettes, including Einweg E-Zigaretten, typically contain fewer known carcinogens than combustible cigarettes, that does not mean they are free of cancer risk. Experts emphasize that reduced exposure is not equivalent to zero risk. When consumers search for “can e cigarette cause cancer” they are usually asking whether long-term use can initiate or promote cancer in humans. The current scientific consensus, as of the most recent high-quality reviews, is that: vaping exposes users to potentially harmful substances, including some carcinogens at lower levels than cigarette smoke; definitive long-term human data are limited because e-cigarettes are relatively new; mechanistic and animal studies suggest plausible pathways by which some constituents could increase cancer risk over time.
What the evidence says: toxicants and dose
The aerosol from electronic nicotine delivery systems can contain a mix of chemicals. Notable groups include carbonyls (e.g., formaldehyde, acetaldehyde), volatile organic compounds, tobacco-specific nitrosamines (TSNAs) at much lower concentrations than in smoke, metals (nickel, chromium, lead), and flavoring-derived irritants. The risk of carcinogenesis depends on cumulative dose, chemical identity, and exposure duration. Epidemiological studies directly linking e-cigarette use with cancer incidence are still emerging; latency for many cancers is long, and robust large-cohort results will take time.
Laboratory data: in vitro and animal models show that certain e-liquid components and aerosols can damage DNA, induce inflammation, and affect cellular pathways associated with cancer. However, translating these findings to human risk requires caution: exposure levels, modes, and durations differ.
Comparative risk: vaping versus smoking

Health agencies frequently state that for adult smokers switching completely to vaping, overall exposure to many carcinogens and toxicants is substantially reduced compared to continued cigarette smoking. This is the core harm-reduction argument. It is not a declaration of safety. For non-smokers, starting to vape is not recommended because it introduces new exposures and addiction risk. For youth, the precautionary principle applies strongly: avoid initiating nicotine use through Einweg E-Zigaretten or other e-devices.
What health experts emphasize when answering “can e cigarette cause cancer”
- Current smokers who cannot quit should consider switching to less harmful alternatives under clinical guidance.
- Non-smokers, especially adolescents and pregnant people, should not use e-cigarettes.
- Regulation, product standards, and reliable labeling are key to reducing unnecessary exposures.
Factors that influence potential cancer risk from electronic aerosols
Risk modifiers include:
- Device temperature: Higher coil temperatures can increase generation of carbonyls such as formaldehyde, a known carcinogen.
- Liquid composition: Certain flavoring chemicals and solvent impurities can form toxic by-products when heated.
- Frequency and duration of use: Greater cumulative exposure likely raises risk.
- Dual use with cigarettes: Many people use both products, negating potential exposure reductions.
Industry variability and counterfeit products
Because manufacturing standards vary, some Einweg E-Zigaretten sold in unregulated markets may contain unexpected contaminants, unsafe batteries, or mislabeled nicotine content. These factors complicate the ability to generalize about safety and underline the need for regulated manufacturing, testing, and transparent ingredient disclosure.
How to evaluate claims and prioritize safety
When assessing statements about vaping health effects, ask:
- Is the claim based on high-quality human studies, or primarily on laboratory/animal data?
- Are exposure levels comparable to real-world use?
- Does the source disclose conflicts of interest (industry funding)?
Public-health agencies and independent researchers provide more reliable guidance than marketing materials from manufacturers.
Practical harm-reduction and risk-minimizing guidance
For adult smokers considering a switch: consult healthcare providers about cessation options. If choosing a vaping product as a transitional tool, prefer regulated products with clear ingredient lists, avoid modifying devices, and use the lowest effective nicotine dose to manage cravings. For parents and educators: secure devices out of reach, educate youth about addiction and chemical exposure, and advocate for flavored-product restrictions that target youth uptake.
Regulation, testing, and product standards
Strong regulatory frameworks can reduce unnecessary exposures by setting maximum limits for contaminants, requiring batch testing, and enforcing accurate labeling for nicotine content. Many countries have introduced product standards specific to Einweg E-Zigaretten and e-liquids, focusing on child-resistant packaging, toxicant limits, and marketing restrictions to protect adolescents.
What ongoing research is focusing on
Research priorities include large-scale prospective cohort studies to track cancer incidence among long-term exclusive vapers, mechanistic studies identifying which chemicals or mixtures drive carcinogenic processes, and comparative toxicology that quantifies risk differences between products and usage patterns. Surveillance for new products and novel chemical ingredients is also critical.
Reliable resources and where to read more
When researching whether “can e cigarette cause cancer” look for peer-reviewed systematic reviews, statements from independent public-health organizations, and government risk assessments. Avoid drawing definitive conclusions from short-term product marketing or single small laboratory studies.
Clear practical takeaways
Einweg E-Zigaretten reduce exposure to some known tobacco smoke carcinogens compared with smoking, but they are not free from potentially carcinogenic compounds; the long-term human cancer risk remains uncertain due to limited longitudinal data. Consequently:
- Non-smokers should not start vaping.
- Smokers should prioritize quitting via proven methods; vaping may be an interim harm-reduction strategy for some under clinical advice.
- Regulation and quality control are essential to minimize avoidable risks.

Daily practice tips for clinicians and consumers
Clinicians should ask patients about all nicotine product use, including Einweg E-Zigaretten, offer evidence-based cessation options, and counsel on relative risks. Consumers should keep device batteries safe, avoid modifying hardware, prefer standardized products, and seek professional support when trying to stop nicotine entirely.
Communication and public messaging
Messaging should be accurate and nuanced: highlight reduced exposure potential for current smokers while strongly discouraging initiation among non-smokers and youth. Clear language is more effective than absolutes—phrases like “safer than smoking but not safe” better capture current evidence than simplistic claims.
Concluding expert perspective on “can e cigarette cause cancer”
Most health experts respond that while the absolute causal link between vaping and human cancer needs further long-term study, there is credible biological plausibility and evidence of exposure to carcinogens in e-cigarette aerosol. Therefore, caution is justified, regulatory oversight is needed, and public-health strategies should prioritize cessation for smokers and prevention of youth uptake.
Appendix: quick reference checklist
- Are you a non-smoker? Do not start vaping.
- Are you a smoker seeking to quit? Discuss options—nicotine replacement therapy, medications, counseling, and, in some cases, supervised switching to regulated vaping products may be considered.
- Concerned about product safety? Buy regulated brands sold through licensed vendors and avoid tampering with devices.
FAQ
Q1: Is vaping completely safe compared to smoking?
No. While many hazardous compounds are present at lower levels in e-cigarette aerosol than in tobacco smoke, vaping is not risk-free and long-term cancer risk remains uncertain.
Q2: Can children be harmed by exposure to secondhand aerosol from disposable vapes?
Secondhand aerosol contains nicotine and other chemicals; minimizing exposure, particularly for children and pregnant people, is recommended.
Q3: Do flavorings increase cancer risk?
Certain flavoring chemicals can produce toxic by-products when heated; some have been associated with cellular toxicity in studies. More research is needed to quantify long-term risks.

Q4: What should I do if I want to quit nicotine?
Consult healthcare providers for evidence-based cessation programs, which may include counseling, nicotine replacement therapies, and medications. Behavioral support improves success rates.
This content synthesizes current knowledge into an accessible format for readers searching for reliable answers about disposable e-devices and cancer risk. It aims to promote informed personal decisions and public-health dialogue rather than provide medical diagnosis. For personalized medical advice, always consult a licensed clinician.